June 8, 2018
‘Uber’ drug delivery for cancer patients
Taking a closer look at the future of delivering drugs directly to the tumour site with implantable devices
Cancer remains one of the major causes of death in Australia, despite improved treatments and rates of survival.
Traditional chemotherapy treatments have proven to have limitations in how effectively they deliver drugs to the tumour site, causing toxicity to healthy tissues, and failing to prevent the disease reoccurring.
However, advances in implantable drug delivery systems (DDS) means targeted treatments to the tumour site are showing promise as a more effective alternative to chemotherapy.
“It’s a bit like hiring an uber driver, the biopolymer is effectively behind the wheel delivering a treatment. Local drug delivery is more effective and can diminish the negative side effects of chemotherapy and improve a patient’s quality of life,” said PhD candidate Sepehr Talebian.
Implantable DDSs contain one or more drugs and are placed around or inside the tumour to directly target the cancerous cells. Other DDSs treat sites where tumours have been removed to prevent the cancer from reoccurring.
Over the past decade a wide variety of biomaterials (materials which interact with living cell systems) have been used to test which is most effective for targeted drug delivery.
In the recently published review, , researchers from the (IHMRI), the (ACES) and the ¡Ò¡´ ”∆µapp of ¡Ò¡´ ”∆µapp (UOW) looked at the pros and cons of a variety of DDS biomaterials trialled.
The review paper’s lead authors, Dr , Senior Research Fellow at ACES and at UOW’s Intelligent Polymer Research Institute and an honorary Emerging Research Fellow at IHMRI, and Distinguished Professor (Director of ACES) have been working for a number of years on developing innovative controlled drug delivery strategies.
“Having precise control over where and when the drug is delivered means you can significantly reduce the drug dosage that is required – and thereby reduce the side effects – and also maintain the delivery of the drug over a longer duration of time,” Dr Foroughi added.
Working with colleague Dr , along with international collaborator Professor Dolatshahi-Pirouz (Technical ¡Ò¡´ ”∆µapp of Denmark), the team are creating the next generation of biopolymers for localising drug delivery systems.
“Biopolymers provide an ideal platform for implantable DDSs because as they can be rendered biodegradable, therefore they do not need to be surgically extracted after use as they can be cleared naturally by the body,” said Dr Foroughi.
The review paper described most recent developments and applications of biopolymer-based implantable DDSs for cancer treatments, focusing on the studies that were further down the path in making the transition from concept to clinical application.
It also described how DDSs have shown immense promise in treating malignant tumours by delivering a variety of anticancer therapeutic agents. However, biopolymeric implantable DDSs come up short in treating metastasis and a dual delivery therapy that combines DDSs with conventional chemotherapy is vital to approach cancer from all sides.
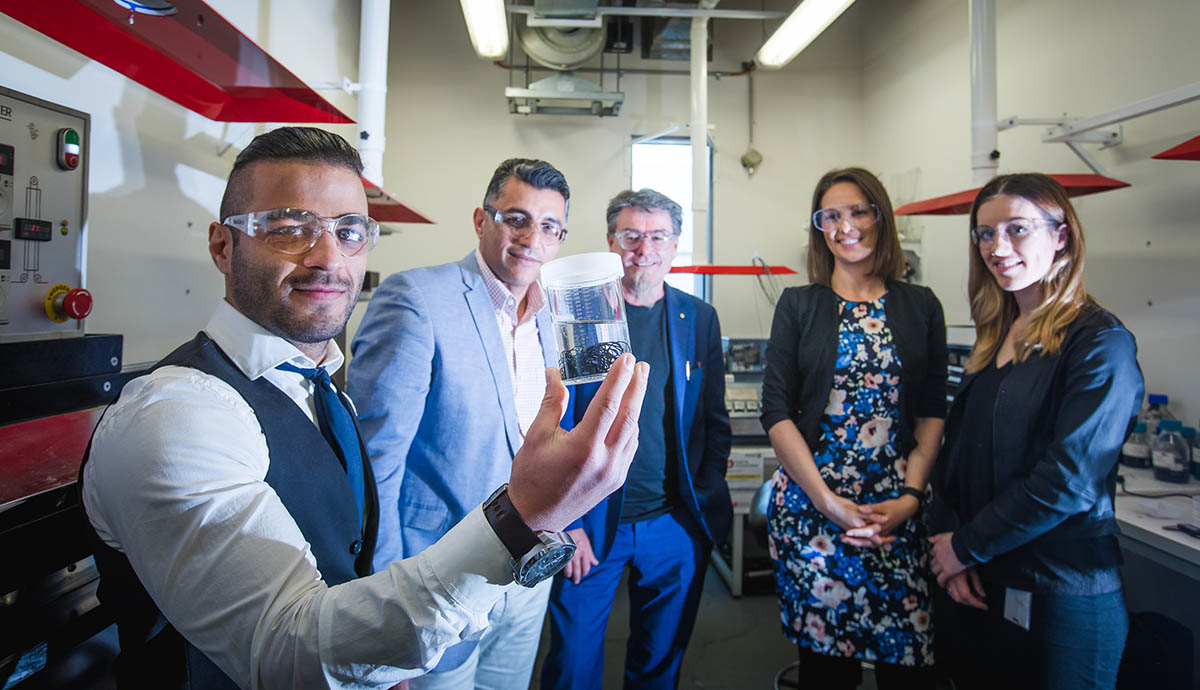
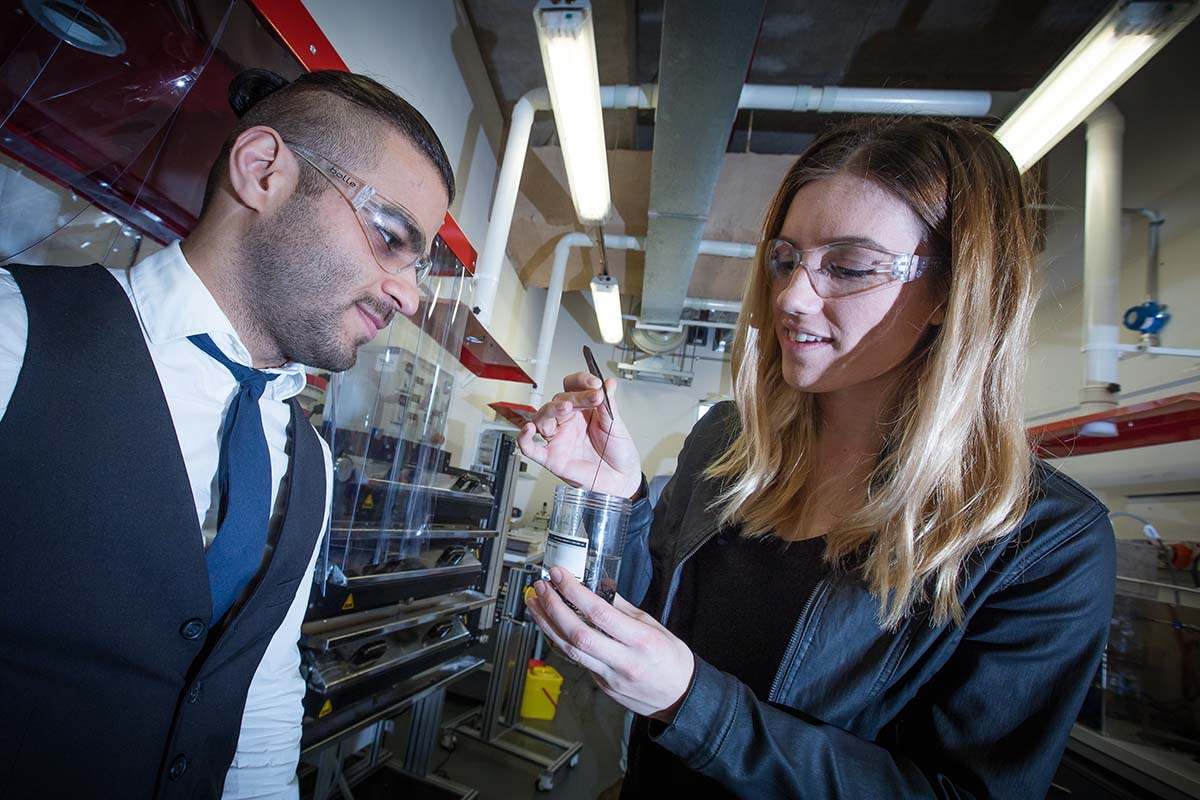
(Main image: PhD candidates Samantha Wade and Sepehr Talebian, Dr Javad Foroughi, Distinguished Professor Gordon Wallace and Dr Kara Vine-Perrow. Picture: Alex Pike.)